Colon Cancer
What is the Colon ( Large Intestine )?
The large intestine – also called the colon, is about 1.5 meters long muscular tube- the last part of the digestive ( Gastrointestinal tract ). The food after being absorbed and digested largely in the small intestine passes into the large intestine, where mainly absorption of water and salt happens. The waste and the remainder is excreted as feces ( stool ).
The colon commences once the small intestine ends and the junction is marked by the presence of the appendix. The colon has different sections ( segments ). The last part of the colon is called the rectum, which itself terminates on the exterior through the anal canal.
The colon has a rich network of blood vessels supplying it and also has a rich lymphatic drainage, which drains into various lymph nodes located in different territories around the colon through the abdomen.

LARGE INTESTINE CANCER [ COLON CANCER ] – ADENOCARCINOMA
In recent times there has been an increase in the incidence of cancers of the colon.
- Almost 10% of cancer cases worldwide are Colon Cancer.
- It’s the 3rd most common cancer in men and 2nd most common cancer in women.
- Increasing urbanization and “western lifestyle” are possibly related to an increased incidence of colon cancer. hence there has been an increase in this cancer in India and in areas, where previously the incidence was low.
- About 5% of all colon cancer cases are hereditary/genetic/familial. these run in families and can be detected very early through colonoscopy and other screening methods.
- Colon Cancer treated properly and in time leads to cure.
RISK FACTORS FOR DEVELOPMENT OF COLON CANCER
1. AGE
Generally speaking the risk of developing colon cancer increases with age. However, colon cancer is increasingly being seen in younger individuals also. Many of them have familial ( genetic ) colon cancer.
2. FAMILY HISTORY AND INHERITED SYNDROMES
Some genetic conditions ( Lynch Syndrome, HNPCC ) – put individuals at a higher risk of colon cancer. These are transmitted through genes in the family and hence put individuals at an increased risk of developing cancer. Not all individuals with these genes will however develop the cancer. Knowledge of genetic transmission can lead to early screening and early detection.
3. POLYPOSIS SYNDROMES / FAMILIAL POLYPOSIS SYNDROMES
Some specific syndromes result in the formation of polyps ( small growths ) in the colon, which are called polyposis syndromes. these are also transmitted genetically and patients run an increased risk of colon cancer and certain other cancers ( colon, fibromas, Desmoid tumours, brain tumours, colon, pancreas and biliary tree ). Such syndromes include Familial Adenomatous Polyposis, Gardners Syndrome, Turcot Syndrome. Patients develop colon cancer at a very young age ( 35-40 years ).
4. ULCERATIVE COLITIS
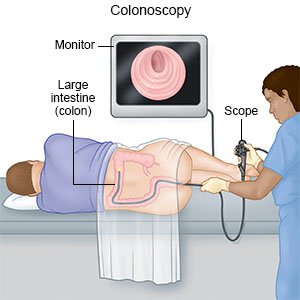
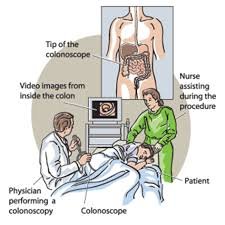
Ulcerative colitis, when present for 10 years or more, increases the risk of development of colon cancer. Patients with ulcerative colitis need regular surveillance colonoscopy and biopsies to see if a cancer is developing. In high-risk patients, surgery will be required before cancer develops.
5. COLON POLYPS
Isolated polyps of the colon also increase the risk of colon cancer. Patients who have had polyps discovered in the colon need periodic and regular surveillance colonoscopy.
6. SMOKING
7. OBESITY
May be associated with an increased risk of developing cancer, especially in the upper part of the colon
8. SEDENTARY LIFESTYLE – LOW PHYSICAL ACTIVITY
9. LOW FIBRE HIGH FAT DIET
The typical western diet which is rich in fat and low on fibre puts individuals at an increased risk of colon cancer. Having in a diet rich in meat – especially red meat and processed meat also increases the risk.
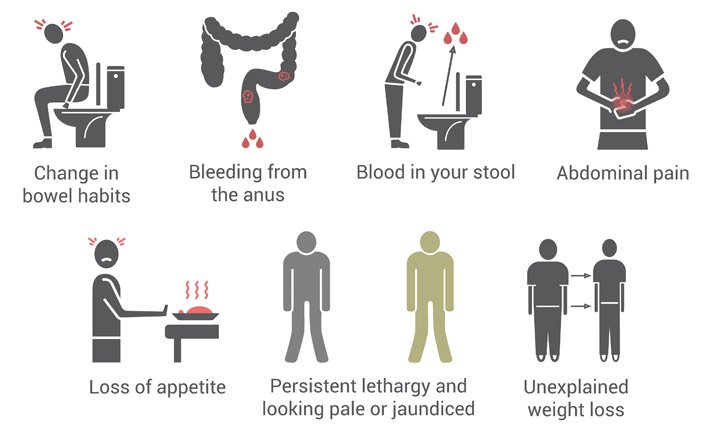
What are the common symptoms of Colon Cancer?
1. Abdominal pain – discomfort in the colon/abdomen including cramps and feeling of tightness
2. A recent change in bowel habits- increasing constipation or alternating constipation and diarrhoea
3. Unexplained weight loss
4. Presence of anaemia – low haemoglobin on a regular blood test done for some reason
5. Bleeding in the stool – either fresh blood or even altered ( dark – black/brown).
6. Fatigue and tiredness.
7. Nausea.
8. A small proportion of patients with colon cancer present as a surgical emergency – since the tumour within the colon may.
- Cause Intestinal obstruction – blockage to the passage of stool – resulting in distention ( swelling ) of the abdomen, along with significant pain and vommiting – this needs emergency hospitalisation and even an emergency operation
- Bleeding – the tumour may bleed significantly causing loss of blood
- Perforation – occasionally the tumour may rupture within the abdomen causing dangerous and life-threatening infection. am emergency high-risk operation will be required to control the situation.
9. Polyps– patients may undergo colonoscopy for vague and non-specific digestive symptoms. tumours and pre-cancerous lesions ( polyps ) may be discovered during scopy. a biopsy will confirm the diagnosis.
DIAGNOSIS OF COLON CANCER
Upon clinical examination and history of the patient, being taken by the related specialist, the diagnosis is made on,
Radiological Imaging
Either Ultrasound, CT scan, and MRI scans. Precise staging and defining the treatment requires accurate and detailed imaging which can be done only via CT scan and MRI.
PET-CT Scan
A FDG PET / CT scan will be required to determine the local extent of spread and to identify if the disease has spread into the rest of the body.
Tumour Marker – CEA
This is a simple blood test – measuring the level of the Carcinoembryonic Antigen ( CEA ) helps make a diagnosis. In most cases, the levels are elevated.
There are broadly 4 stages for colorectal cancer:
Stage I
At this stage, the tumor is limited to the top layer of tissue that lines the inside of the colon. Cancer cells also may have spread to a limited number of nearby lymph nodes.
Stage II
Cancer at this stage has spread deeper, growing into a deep muscle layer of the colon. Cancer may also have spread to more of the lymph nodes.
Stage III
At this stage, the cancer may have grown through all the layers of the colon and spread to nearby structures. Or it may be a smaller cancer that has spread more extensively to the lymph nodes.
Stage IV
This stage indicates that the cancer has spread to distant areas of the body.eg: liver, lungs, bones, etc.
How is COLON cancer treated?
Colon cancer treatment depends on many factors. The three most important aspects which define the course of treatment include
- Stage of the disease – Best defined on CT scan -the CT will also help define other tumour characteristics which define treatment – the size of tumour, location of the tumours, proximity to blood vessels, number of tumours, etc
- Laparoscopy – Sometimes a staging laparoscopy may be required to accurately define the stage of the tumour and help the surgeon plan treatment. This involves a small surgical procedure in the operating room, wherein a camera ( laparoscope ) is inserted into the abdominal cavity and precise information of the tumour is taken. Biopsies of the peritoneum/liver / fluid samples may be taken to help with staging and treatment planning.
- General health and condition of the patient.
Treatment for COLON CANCER :
1. Surgery
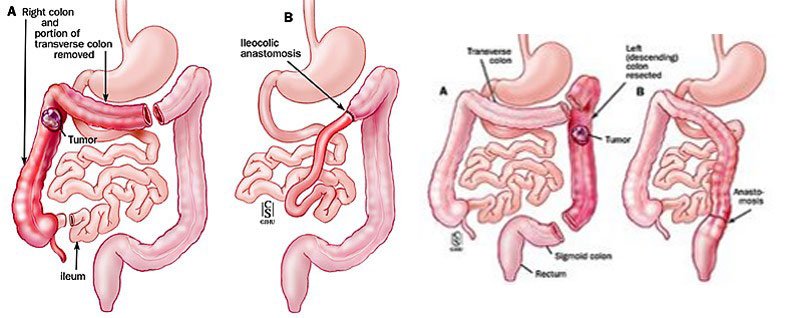
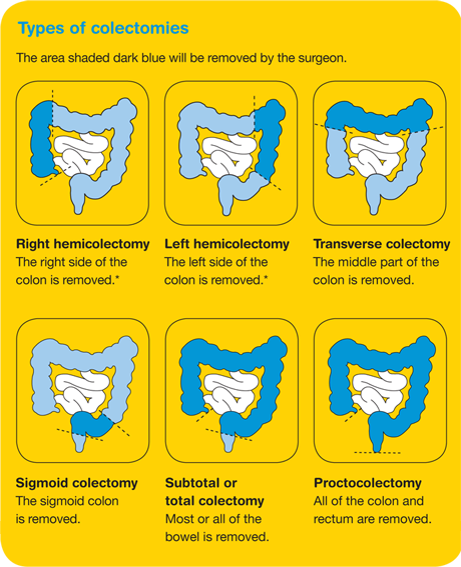
Surgery for adenocarcinoma of the colon includes – removal of part of the colon bearing the tumour with an adequate part of normal ( non tumour ) colon ( to obtain tumour free margin ). Surgery may range from removal of the right colon – right colectomy, left colon – left colectomy, transverse colon- transverse colectomy, sigmoid colectomy and rectal resection.
Upon removal of the colon, the digestive anatomy is restored by joining a part of the two ends of the colon.
All the regional and zonal lymph nodes, within the area of drainage, are removed along with the colon, thereby carrying out a complete radical lymph nodal dissection.
The final stage of the tumour, can be commented upon after detailed histological examination of the removed tumour and lymph nodes.
Surgery may be done through the open technique ( cut on the abdomen ) or keyhole technique ( minimally invasive ) – laparoscopic or laparoscopically assisted methods.
Depending on the stage of the disease ( determined via staging investigations – CT scan / PET scans/laparoscopy), patients may need to take upfront chemotherapy and radiation ( neoadjuvant chemotherapy ), prior to surgery. This will be determined by your treating cancer physician and surgeon. This treatment protocol is more followed in rectal cancer.
2. Chemotherapy
Most patients with colon cancer will require chemotherapy. this may be given either before the surgery ( neoadjuvant ) or following surgery – Adjuvant Chemotherapy
The decision for chemotherapy is taken by the cancer physician and depends on a variety of factors including the general condition of the patient, stage of the tumour, presence of obstruction/bleeding, etc.
This may be used as a neoadjuvant therapy, after surgery alongside chemotherapy. This will depend on the stage of the tumour and judgement of the treating cancer physician. This is particularly so in patients with rectal cancer.
Supportive and Palliative Therapy
- Pain relief with specific pain medications to alleviate pain.
- Relive obstruction – endoscopic placement of a stent or performance of a stoma.
- Prevent vommiting and other symptoms.
- Removal of fluid from the abdomen – ascites tapping.
- Other supportive therapy.
Palliative Surgery
Sometimes palliative surgery will be required. This means the cancer cannot be cured/removed completely but an operation needs to be done to remove the main tumour in the colon which may be.
- causing obstruction
- bleeding
It may also mean to perform a stoma -the diversion of the stool passage on to the skin, through a small bag to relieve the obstruction from the cancer. [ see section on stoma ].
When performing palliative surgery it usually means that the cancer has spread through the body but surgery is required to improve the health of the patient, enable diet, and improve quality of life.
Prevention of Colon Cancer
Colon Cancer is a potentially preventable condition.
A healthy lifestyle, avoidance of alcohol, regular exercise, avoidance of smoking are some basic measures which apart from other health benefits also protect against colon cancer.
Other measures include,
– Regular treatment and follow up in high-risk cases: positive family history, history of colon polyps, genetic transmission, and tests being positive.